Breast Cancer Detection & Diagnosis
Breast cancer rarely shows early symptoms, which is why regular screening is so important. Most women should start getting regular mammograms around the age of 40. Some women who are considered high-risk may need to undergo other types of screening, such as clinical breast exam or MRI. The earlier breast cancer is detected and diagnosed, the easier it is to treat.
Mammogram for Breast Cancer Screening
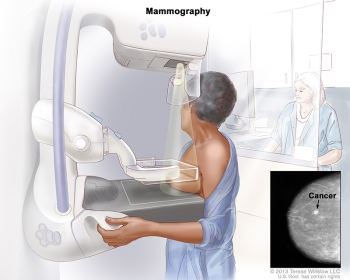
In the past, 2D mammography was the only available option for breast cancer screening. Today, however, women can receive a newer, 3D method of mammography called tomosynthesis. This updated technology differs from standard 2D mammography in that it takes pictures from many angles rather than a single straightforward X-ray image of the breast. This allows for a more comprehensive and in-depth view of breast tissue. While all women can benefit from 3D mammography, it is especially beneficial to those with dense breasts since this technology is more likely to detect lumps than a 2D mammogram would. Talk with your doctor to see what method would be the best for you.
Women are encouraged to begin regular screening mammograms before having symptoms so breast cancer can be caught early. The right time to start breast cancer screening is based on the risk level of each individual patient. The United States Preventive Services Task Force (USPSTF) issued a new draft of recommendations for breast cancer screening:
- Women at average risk of breast cancer should begin breast cancer screening at age 40 instead of the previously recommended starting age of 50
- Screening mammograms should be repeated every other year from ages 40 to 74 for women at average risk
Screening recommendations change for women at a higher risk of developing breast cancer. All women should understand what to expect when getting a mammogram for breast cancer screening – what the test can and cannot do. It’s important to consult with your doctor to determine a screening plan that’s best for you.
Clinical Breast Exams (CBE) and Breast Self-Exam (BSE)
Because mammograms are so effective, clinical breast exams or breast self-exams are not usually recommended as part of a routine breast cancer screening schedule for average-risk women. However, women at higher-than-average risk may want to talk to their doctor about whether a clinical breast exam would benefit them.
During a clinical breast examination, your physician will thoroughly check your breasts. You may be asked to raise your arms over your head, let them hang by your sides, or press your hands against your hips.
Your healthcare provider will look for differences in the size or shape of the breast as well as changes in the skin of the breasts and nipples. They will carefully feel your breasts, under your arms, and along your collarbone area for any abnormalities, such as a lump or enlarged lymph nodes. Your nipples may be squeezed to check for fluid.
If a lump is found, your doctor will feel its size, shape, and texture. They will also check to see if the lump moves easily. Benign (non-cancerous) lumps often feel different from cancerous ones. Lumps that are soft, smooth, round, and movable are likely to be benign. An oddly shaped lump that feels hard and firmly attached to the breast is more likely to be cancer, but additional testing is needed to confirm a diagnosis.
In general, all women should be familiar with how their breasts normally look and feel and should report any changes to a healthcare provider right away.
Additional Imaging for Women at High Risk
Women who are at high risk for developing breast cancer should begin breast cancer screening earlier than those considered average risk. Your doctor may recommend that you get a breast MRI in addition to a mammogram every year starting at age 30. High-risk individuals include women who:
- Have a family history that indicates a higher lifetime risk of developing breast cancer
- Have a known BRCA1 or BRCA2 gene mutation based on genetic testing
- Have a first-degree relative (parent, brother, sister, or child) with a BRCA1 or BRCA2 gene mutation and have not had genetic testing themselves
- Received radiation therapy to the chest when they were between 10 and 30 years of age
- Have Li-Fraumeni syndrome, Cowden syndrome, or Bannayan-Riley-Ruvalcaba syndrome, or have first-degree relatives with one of these syndromes
Breast Biopsy
A biopsy is the removal of breast tissue to determine if cancer cells are present. It is the only way to confirm a breast cancer diagnosis. A sample of fluid or tissue from your breast can be taken in several different ways, including:
- Fine-needle aspiration biopsy: A thin needle is used to remove cells or fluid from a breast lump.
- Core biopsy: A sample of breast tissue is extracted with a wide needle.
- Skin biopsy: A small sample of skin is taken if there are noticeable skin changes on the breast.
- Stereotactic biopsy: a radiologist or breast surgeon uses a hollow needle to remove samples of tissue from the breast mass. This procedure uses a mammogram to determine the location of suspicious areas in the breast.
- Surgical biopsy: This procedure uses surgery to remove all or part of the abnormal area found in the breast.
Watch the video below to learn facts about a breast biopsy. The video discusses what a breast biopsy is, the different types of breast biopsies, the reasons for needing one, and what to expect after the biopsy.
The sample removed from your breast will be examined by a pathologist who will record the findings in a pathology report. If cancer is detected, the pathologist will determine the type of breast cancer. Your oncologists will use this report to help determine the best next steps.

 Learn More
Learn More